The global fight against cervical cancer has reached a watershed moment with the World Health Organization (WHO) releasing groundbreaking data showing that new vaccines can reduce incidence rates by an astonishing 90%. This development marks a turning point in women's health, offering hope for the eventual eradication of what has long been one of the most preventable yet persistent cancers affecting women worldwide.
For decades, cervical cancer has remained a stubborn public health challenge, particularly in low- and middle-income countries where screening programs are limited. The WHO estimates that cervical cancer claims over 300,000 lives annually, with nearly 90% of these deaths occurring in developing nations. The introduction of these highly effective vaccines could fundamentally alter this devastating landscape, potentially saving millions of lives in the coming generations.
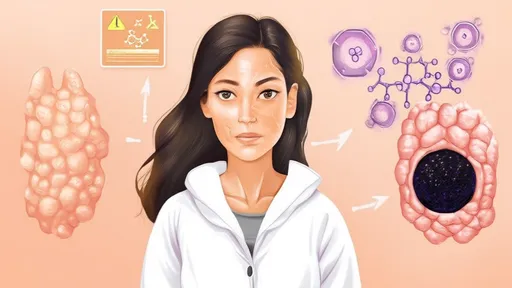
The remarkable efficacy of these vaccines stems from their targeted approach against human papillomavirus (HPV), the primary cause of cervical cancer. Unlike previous versions that protected against fewer HPV strains, the new generation of vaccines provides broader coverage against the most dangerous cancer-causing variants. Clinical trials have demonstrated unprecedented success in preventing not just HPV infection but the subsequent development of precancerous lesions that lead to cervical cancer.
Public health experts are particularly encouraged by the vaccine's performance in real-world settings, where effectiveness often differs from controlled trial conditions. Population studies across multiple continents have consistently shown the 90% reduction figure holding true across diverse genetic backgrounds and living conditions. This consistency suggests the vaccine's benefits could be universally applicable, provided adequate vaccination coverage can be achieved.
The implications of this medical breakthrough extend far beyond individual health outcomes. Economists project that widespread vaccination could save healthcare systems billions in screening and treatment costs while preserving workforce productivity. In many developing countries where cervical cancer often strikes women during their prime working years, the socioeconomic impact could be transformative for families and communities.
However, significant challenges remain in translating this scientific triumph into global health equity. Vaccine distribution networks in resource-limited settings often struggle with cold chain requirements, while cultural barriers and misinformation continue to hinder acceptance in some regions. Health authorities emphasize that the full benefits will only materialize through sustained investment in healthcare infrastructure combined with community education programs.
The WHO has responded by accelerating its cervical cancer elimination strategy, setting ambitious targets for vaccination coverage alongside improved screening and treatment protocols. Several countries have already reported dramatic declines in HPV prevalence following successful vaccination campaigns, providing early validation of the strategy. These successes are fueling optimism that with sufficient political will and international cooperation, cervical cancer could follow smallpox into the history books.
As vaccination programs expand, researchers are already observing promising secondary effects. Early data suggests the vaccines may also reduce rates of other HPV-related cancers affecting both men and women, including certain oral and anal cancers. This unexpected bonus could further enhance the vaccines' public health value and strengthen the case for universal access.
The development stands as a testament to decades of medical research and international collaboration. From the initial discovery of HPV's role in cervical cancer to the painstaking vaccine development process, this achievement represents one of modern medicine's greatest success stories. For the millions of women at risk worldwide, it offers not just protection from disease but the promise of longer, healthier lives free from the shadow of cervical cancer.
While celebrating this progress, health leaders caution that vaccines alone won't complete the elimination agenda. They stress the continued importance of screening programs to catch cases in unvaccinated populations and the need for ongoing research into even more accessible vaccine formulations. The coming years will prove critical as nations work to implement comprehensive strategies that combine vaccination with other proven interventions.
For healthcare professionals on the frontlines of cancer prevention, the new data provides powerful ammunition in their efforts to combat vaccine hesitancy. The dramatic efficacy figures make a compelling case for prioritizing HPV vaccination in national immunization schedules and removing barriers to access. Many are hopeful that the stunning 90% reduction figure will finally push cervical cancer prevention to the top of global health agendas.
The psychological impact on women's health cannot be overstated. In cultures where cervical cancer carries particular stigma, the prospect of near-complete prevention could encourage more open discussions about reproductive health. Patient advocates report that the vaccine's success is already changing how young women and their families perceive their cancer risk, fostering a new sense of empowerment and control over their health destinies.
As implementation challenges are addressed, attention is turning to the long-term implications of such effective prevention. Epidemiologists are beginning to model how drastically reduced cervical cancer rates might reshape women's healthcare in future decades, with some speculating about possible reallocation of screening resources to other health priorities. Such projections, while preliminary, underscore the transformative potential of this medical breakthrough.
The story of cervical cancer vaccination serves as a powerful reminder of what global health initiatives can achieve when science, policy, and compassion converge. As vaccination rates climb and incidence rates fall, the world may soon witness the first elimination of a cancer through deliberate public health intervention—a milestone that would inspire new ambitions across the entire field of oncology.
By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025