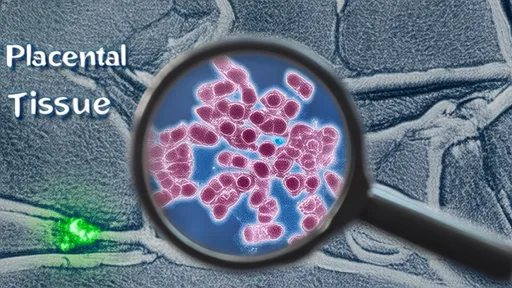
The global health community is facing a growing threat from Candida auris, a drug-resistant fungus that has shown alarming resilience against existing treatments. First identified in 2009, this so-called "superbug" has since spread across multiple continents, challenging healthcare systems with its ability to evade conventional antifungal medications. Unlike other fungal pathogens, C. auris resists elimination through standard sterilization protocols, allowing it to persist on surfaces and medical equipment for extended periods.
What makes Candida auris particularly concerning is its rapid development of resistance to all three major classes of antifungal drugs: azoles, echinocandins, and polyenes. Recent studies reveal that some strains now demonstrate resistance to multiple drug classes simultaneously, leaving clinicians with few therapeutic options. The fungus primarily affects immunocompromised patients, including those in intensive care units, cancer treatment centers, and long-term care facilities, where it can cause bloodstream infections with mortality rates approaching 60%.
The evolutionary trajectory of C. auris resistance appears unprecedented in fungal pathogens. Researchers have identified several mechanisms behind its drug defiance, including enhanced efflux pumps that expel medications from fungal cells and mutations in drug target sites that render treatments ineffective. Compounding the problem, standard laboratory tests often fail to accurately detect resistance patterns, leading to inappropriate treatment choices and further selection pressure for resistant strains.
Environmental factors may be accelerating this resistance crisis. The widespread use of fungicides in agriculture, particularly those chemically similar to medical antifungals, has created selective pressure that primes fungal populations for drug resistance before they even encounter clinical settings. Climate change may also be playing a role, as rising temperatures potentially allow fungi like C. auris to adapt to mammalian body temperatures—a historical barrier that protected humans from most fungal infections.
Public health responses have struggled to keep pace with the evolving threat. Many countries lack robust surveillance systems to track C. auris cases, and infection control protocols vary widely between institutions. The COVID-19 pandemic exacerbated the situation, diverting resources from fungal surveillance and potentially facilitating undetected spread through overwhelmed healthcare systems. Some researchers speculate that the increased use of broad-spectrum antibiotics and steroids during the pandemic may have created more favorable conditions for C. auris colonization and infection.
Innovative approaches are emerging to combat this resilient pathogen. Scientists are exploring combination therapies that pair existing antifungals with adjuvants to overcome resistance mechanisms. Other promising avenues include the development of antifungal stewardship programs, novel drug formulations like lipid-based amphotericin B, and investigational compounds that target different fungal pathways. Diagnostic improvements, particularly rapid molecular tests that can identify resistance markers within hours rather than days, are also critical for guiding appropriate treatment decisions.
The economic implications of unchecked C. auris spread could be substantial. Extended hospital stays, expensive antifungal treatments, and enhanced infection control measures all contribute to rising healthcare costs. In low-resource settings where diagnostic capabilities and treatment options are limited, the impact could be particularly severe. Some estimates suggest that antimicrobial resistance overall could cost the global economy up to $100 trillion by 2050 if current trends continue, with C. auris representing a growing portion of that burden.
Addressing the C. auris challenge requires coordinated international action. This includes strengthening global surveillance networks, investing in antifungal research and development, and implementing stricter regulations on agricultural fungicides that may contribute to medical resistance. Public awareness campaigns are also needed to highlight the seriousness of fungal resistance without causing unnecessary alarm. The experience with C. auris serves as a stark reminder that pathogenic microbes continue to evolve in unexpected ways, demanding constant vigilance and innovation from the medical and scientific communities.
Looking ahead, researchers emphasize the need for a paradigm shift in how we approach fungal infections. Rather than reacting to resistant strains as they emerge, proactive measures such as environmental monitoring of healthcare facilities and development of antifungal vaccines could help prevent resistance from developing in the first place. The story of Candida auris is still being written, but its rapid rise and adaptability underscore the urgent need for new strategies to protect public health in an era of increasing antimicrobial resistance.
By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025
By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025

By /Jul 25, 2025